Last updated:
‘From Mental Hygiene to Community Mental Health: Psychiatrists and Victorian Public Administration from the 1940s to 1990s’, Provenance: The Journal of Public Record Office Victoria, issue no. 7, 2008. ISSN 1832-2522. Copyright © Belinda Robson.
This is a peer reviewed article.
This paper offers an overview of public policy in Victoria as it changed its approach to the treatment and prevention of mental illness from the late 1940s to the 1990s. While this has come to be understood as a move away from institutional to community care, I argue that there is still a great deal to understand about how government policy managed this process and how the concepts beneath community mental health have been applied. In this paper I look at the role of psychiatry and suggest that during this period there were a range of ways psychiatrists came to influence public policy. I pay particular attention to the perspectives of the first chairman of the Mental Hygiene Authority, the psychiatrist Eric Cunningham Dax (1908-2008). I hope to offer insights into the way debates and perspectives about mental health evolved in Victoria by looking at government archives from the period and contextualising them within the internal debates within psychiatry. There are three factors that are suggested as defining features in this policy environment. The first was the move in the locus of treatment from a hospital setting to a community setting, fuelled by improved medication and the high costs of maintaining old and large separate institutions. The second was the changing role of psychiatrists, in response to their increased role in the community. The third was the administrative amalgamation of health and mental health from the 1970s which enabled a generic model of health promotion to become a public policy priority.
The paper draws on the available public records to describe the story of how government modified its approaches over time. Records which reflect these policy debates have been accessed through Public Record Office Victoria, the Department of Human Services, and the Royal Australian and New Zealand College of Psychiatrists. It concludes with a recommendation that further research be conducted in this area across State and Commonwealth governments to identify how government achieved a shift in mental health care into the community and what this meant for services, staff and patients.
Introduction: Government, Psychiatry and Community Mental Health
This paper looks at some of the issues debated by government and psychiatry as they formulated and implemented mental health policy in Victoria during the past fifty years. It tells the story by picking up various themes along the way: the Mental Hygiene Authority and its role in mental health education; social psychiatry and anti-psychiatry; the administrative amalgamation of mental health into the Health Commission; and the entry of psychiatric terms into broader public discourses about mental illness and its place in society. It is based on available files from Public Record Office Victoria (PROV) as well as the Royal Australian and New Zealand College of Psychiatrists, Annual Reports and the Department of Human Services. While a significant proportion of the Victorian State Government archives held by PROV which relate to policy development in psychiatric services over the last fifty years are closed to the public under the privacy provisions of Section 9 of the Public Records Act 1973, it is still possible to produce a picture of some of the public policy debates around mental health during this period.[1]
The General Correspondence Files (Mental Health), which currently cannot be viewed without special permission, appear to contain many of the internal files on community mental health centres, administration and staffing. A subject card index is available, and this gives an idea of the areas of policy under consideration by government. The closure of all records which relate to service development is because records may reveal personal details of patients and their families. There are therefore voices in this story which for the current time remain unheard, especially those of patients, carers and staff in the services. This article is intended to further knowledge about how government and psychiatry related to each other – just one layer in what has to be a very complex picture of social and cultural change.
The philosophical debates which characterised policy around mental health and mental illness from the 1950s onwards resulted in a split between two policy objectives. The first objective was to design services for the treatment of mental illness in individuals that met the needs of a community-based rather than an institution-based service system. The second objective was to make the community itself a site where psychiatric concepts were readily understood and integrated into the social fabric of everyday life.
For the new service design to be successful, families and other immediate networks had to be able to identify symptoms of mental illness, evaluate their severity, feel prepared to seek assistance and, if necessary, seek admission of patients to hospital as well as readily receive them again after discharge. This required expertise which I will describe as ‘mental health literacy’. The direction of policy attention moved away from the focus on institutions as being separate and largely disconnected from people’s day-to-day lives, and increasingly toward a concept of mental health which attempted to make psychiatric concepts more easily understood by the general community.
Three Paradigms: Treatment, Prevention and Mental Health Promotion
Within the policy setting, three concepts can be inferred from the term ‘mental health’ as it was used by psychiatrists and government officials: mental illness treatment, mental illness prevention, and mental health promotion. These concepts were not mutually exclusive and often overlapped in practice, but for the purpose of this paper they will be treated as separate areas within the historical evolution of policy and practice. The first concept (treatment) refers to the ways people with a diagnosed condition received ongoing clinical care, the second (prevention) has a dual focus on identifying groups at risk of developing mental illness as well as on the factors which contribute to mental illness, and the third (mental health promotion) looks beyond an absence of mental illness and toward social and emotional well-being as its goal. All of these concepts involve a philosophical position about the relationships between the individual, their mental illness, and the role of the broader social and cultural context in creating, managing and preventing illness. How should a mental health system incorporate the various perspectives? What role should government play in mental health prevention and promotion?

In the 1950s and 1960s, the Victorian Mental Hygiene Authority (later the Mental Health Authority), led by the English psychiatrist Eric Cunningham Dax, combined the role of treatment with an active program to build a community with better mental health literacy. It sought to instil a sense of community responsibility for the treatment, rehabilitation and prevention of mental illness. This period saw government begin to take the lead in developing specialised mental health initiatives, closely aided by psychiatrists. From the 1970s, there was a move to integrate the administration of Victoria’s mental health services with other health services, a trend which became more pronounced during the 1980s and 1990s. This move saw psychiatry redefine its parameters in relation to new professional groups. There was a redesign of treatment services away from isolated institutions where patients stayed for many years, and toward day hospitals, community rehabilitation services, and employment and housing support designed to prevent the need for hospital care.
The distinction between treatment and prevention has become recognised within the mental health industry as creating two tangible professions which, while overlapping, need to be treated as separate streams.[2] Some have argued that with limited and inadequate resources for programs to treat and support people with mental illness, there has been a steady decline in the image of public psychiatry.[3] The impact of a split between mental health promotion and mental illness treatment on the lives of people with mental illness is not clear, but with limited resources in the health budget it is arguable that the treatment and care of people with mental illness has had to compete with mental health promotion for attention and resources. But how did this happen and why? How did the policy debates shape community treatment? In order to understand this process, it is necessary to start with the late 1940s when Victoria’s mental health administration underwent a significant overhaul.
The Mental Hygiene Authority and the Creation of Mental Health Literacy
In the late 1940s and early 1950s there were high hopes that mental illness could be reduced through public educational activities. There were also wider social movements to create a society in which mental illness might actually not occur. The World Federation for Mental Health (WFMH) was formed in 1948 by the World Health Organisation and heralded a new era of post-war optimism that society could be re-built to prevent war. The goals of the WFMH included world peace, and its founding document ‘Mental Health and World Citizenship’ claimed that ‘the ultimate goal of mental health is to help [people] live with their fellows in one world’.[4] According to the WFMH, ‘mental health’ could be achieved through global harmony.
While lofty ideals were being articulated on the world stage, psychiatry in Victoria was establishing itself as a profession that could lead policy on mental illness treatment and prevention. During early attempts to professionalise psychiatry, the Australian Association of Psychiatrists (AAP), the precursor of the Royal Australian and New Zealand College of Psychiatrists (RANZCP), began to consider questions of mental health literacy. In 1948 it formed a sub-committee to ‘investigate the possible avenues of propaganda in education in the matter of mental hygiene’.[5]
The AAP also expressed a tendency to ascribe greater levels of mental illness to migrants, reflecting notions of eugenics which characterised the period.[6] The post-war era was one in which homogeneity and social assimilation characterised policy around race, ethnicity and other difference.[7] Indeed, the growing desire to return psychiatric patients to their families and community also reflected this interest in reducing the differences between people with mental illness and those without, by assimilating groups which had previously been separated back into society.
Psychiatrists sought to define themselves as the experts in this process. In 1948 the AAP minutes also recorded that ‘the question of specialization and protection of the term “psychiatrist” was discussed and the Council resolved that steps should be taken to ensure if possible that only medical men be permitted to use the term “psychiatrist”‘. These twin concerns about community education and the professional specialisation of psychiatry characterised the development of mental health services in Victoria over the next fifty years.
The Mental Hygiene Authority (MHA) was established by statute in 1950 as the government body with responsibility for managing the psychiatric hospitals. This body was to replace the Mental Hygiene Department, and it changed its name to the Mental Health Authority in 1959. Despite codifying its administrative responsibility for managing the public psychiatric system, the Mental Hygiene Authority Act 1950 (Vic) also specified that the functions of the MHA included ‘provision for the treatment and measures for the prevention of mental defect disorder and disease’ (Section 10a). Hence prevention was included within its purview, giving legitimacy to its attempts to influence public policy around the social determinants of mental illness.
The psychiatrist Eric Cunningham Dax was brought out by the Victorian Government from England to chair the MHA after a series of inquiries and press-led campaigns about the impoverished state of Victoria’s psychiatric hospitals. Alexander Kennedy of Durham University had conducted an inquiry in 1949 which found that the existing administrative arrangements were no longer effective and that a Mental Hygiene Authority was required that would have six to eight members from diverse professions. When the government decided to have a three-member authority instead, Kennedy wrote to the Minister for Health, CP Gartside, to express his dissatisfaction with this structure and express his view that the chairman should be a lay citizen with ‘energy and experience’ rather than a psychiatrist.[8] Nevertheless, the appointment of Dax as chairman of a three-person authority went ahead. Dax was selected from a total of seventeen applicants, eight from the United Kingdom and nine from Australia. The selection panel was constituted of RD Wright, Dean of Medicine at Melbourne University, JG Hayden from the British Medical Association, and John F Williams, representing the AAP.[9]

There was a clear government preference for a psychiatrist to lead the MHA, indicating its trust in the profession to lead the reform of mental health services. Moreover, the MHA would report directly to the Minister for Health, thus bypassing the bureaucratic tangles which Kennedy had identified as interfering with the autonomy of the former Mental Hygiene Department.
Dax himself was quite suited to working in this environment and immediately began to speak freely to the press, something that his predecessor, John Catarinich, had been constrained in doing in his role as a public servant. When he arrived at the airport, Dax declared to the press: ‘My first objective is to foster a new attitude to mental illness’.[10] The next year he was appealing to the community: ‘The more work there is to be done the better I like it. But please don’t think I’m going to do it myself. It will be done by the staff of your mental hospitals, by social workers and by the public. Unless I can get their help, I’ll be a failure’.[11]
Dax was clearly adept at using the concept of mental health as a means of mobilising reforms that would improve social conditions. In July 1952 he wrote to the Minister of Health, WO Fulton, expressing the view that ‘the attention of the Mental Hygiene Authority [should] be directed to the emergency housing problem with a request that the Authority approach the appropriate ministers to … investigate in detail those aspects of emergency housing camps which bear on the Mental Health of the community’.[12] Housing was not a traditional focus for psychiatry, but here Dax made a clear connection between social conditions and mental health. This foreshadowed the growing interest within government in the links between the environment and mental well-being.
While the mental health of the community was of increasing interest to government, the problem remained that individuals with mental illness required care. The rates of patients entering and leaving hospital were an important barometer of how well the community understood mental illness and to what extent sufferers had sought treatment or were able to be supported outside of hospital. Discharge and admission figures were continually commented upon in the Annual Reports of the Mental Hygiene Authority. In 1955, for example, Dax wrote that the discharge rate had risen from 55 per cent to 71 per cent and that the number of ‘voluntary boarders’ (those who were admitted with the consent of the patient and therefore not needing to be certified by a doctor) had trebled in three years and was running at 40 per cent of all admissions.[13]
In order to improve these figures further, Dax set out to develop prevention programs that targeted individuals at risk of developing an illness. In 1952 he wrote to Fulton requesting funding for a Mental Hygiene Information Bureau ‘for emotional, domestic and psychiatric problems’.[14] The Bureau, he wrote, would be staffed by two social workers and a typist and would ‘ease psychiatric problems of the community’. This service was to provide information to individuals at risk of developing a mental illness. While this particular project was not funded, a similar service was set up as a ‘Personal Emergency Service’ in April 1960, which was staffed by volunteers.[15] The year 1960 also saw the MHA propose a training course in public relations for sections of the staff.[16] A Mental Health Education Officer, Rachelle Banchevska, led many of these activities, and a Mental Health Week became a focus for public education, with exhibitions such as ‘Mental Health – the People’s Wealth’ being held in 1958.[17]
New legislation made the role of government even more clear with regard to both treatment and the building of mental health literacy. The Mental Health Act 1959 (Vic) led to a separation of the mentally ill from the ‘intellectually defective’, provided for ‘easier admission and discharge’, and gave the Authority more power to make arrangements with the Minister for the provision of further community and preventative services.[18] In addition there was to be a greater permeability of the institutions. Admission and discharge would be more streamlined, meaning that the community had to become more literate in mental health in order to recognise when someone should be admitted as well as to be able to receive patients who had been discharged.
Voluntary organisations were critical to this process, both as community educators and in their role providing practical support to patients. The Mental Hospital Auxiliaries, the Melbourne Rotary Club, Victoria’s Aid to the Mentally Ill, the Red Cross and the Country Womens’ Association all played an active role.[19] But while Dax encouraged the public to become more involved with mental health, he also advocated that the psychiatrist should be closely involved in all of the community efforts. Volunteers and social workers had a role to play in mental health promotion, he noted in his 1961 book Asylum to Community, but ‘the psychiatrist should take an active part in community care, the promotion of mental health and the prevention of mental illness’ (p. 30). Dax was a strong voice for his profession and sought to increase the status of psychiatrists within the public sector.
In some ways, the work of the MHA during the 1950s and 1960s benefited from the boom economy of the period, following the climate of post-war reconstruction, expanded social welfare, and expanded notions of social citizenship. Between 1939 and 1956 public employment rose from 67,000 to 154,000.[20] The total combined Commonwealth and State expenditure in health and community services grew from £160,450 in the period 1949-50 to £675,867 in the period 1961-62.[21]
This was also a period that saw increased optimism about the new treatments which enabled patients to leave hospital and use the new outpatient clinics. The project known as ‘deinstitutionalisation’ saw the number of patients in Victorian psychiatric hospitals decline by 33 per cent between 1963 and 1973.[22] ‘Largactil’ (chloropromazine) and lithium were hailed by the psychiatrist JFJ Cade (himself a leading figure in the discovery of lithium) as allowing a ‘multitude of schizophrenics [to be] maintained in the community, at home and working, whereas once they would have been foredoomed to spend the rest of their days as chronic mental hospital patients’.[23] On a similar note, Cade applauded the tri-cyclic anti-depressants and benzodiazepines as contributing to an environment where ‘equanimity [is] brought on by prescription’.[24]
But while psychiatry as an emerging profession was enjoying an increase in status as a result of these modern treatments, there was disquiet within its ranks about other competing professions in the community. For example, in 1959 the AAP discussed the government’s support for Marriage Guidance Councils and clearly felt that it would be better if the government subsidised qualified psychiatric services to perform this role.[25] Psychiatry was keen to work beyond the traditional clinical focus and faced competition from agencies which were supported by the government to work with the community on broader social issues. This created an environment where psychiatry had to clarify its role and defend its expertise.
Social Psychiatry and Anti-Psychiatry
Beginning in the 1960s, there was interest amongst some psychiatrists in conducting collaborative research with a range of professionals including sociologists, psychologists and social workers as well as psychiatrists. As the historian George Rosen commented in 1968, reflecting on whether psychiatrists had a role in public mental health: ‘the problem in mental hygiene is basically one of aetiology’. Therefore, psychiatrists saw themselves as having expertise to offer in determining what caused mental illness. Nevertheless, Rosen also observed that ‘many of the weaknesses in the mental hygiene movement reflect the deficiencies that psychiatrists have brought to it’.[26] It was a time for reflection and the re-orientation of psychiatry if the profession were to build a place for itself in the public dialogue about the cause-and-effect relationships between the environment and mental illness.
The late 1960s saw the partnership between biological and psychological and social approaches strengthen.[27] This was difficult when psychiatry itself was divided about the respective roles of biology and environment in causing mental illness. As David Hamburg noted in 1970, ‘It is no longer worth while to ask, Is schizophrenia genetic or environmental? The basic questions center on the specific nature of the gene-environment’.[28] To add weight to the argument about the relationship between illness and environment, Hamburg cited research ‘a decade ago’ which surveyed people with mental illness to look at whether mental illness was related to class, and found that schizophrenia was more prevalent in lower classes. It also found that patients from the upper classes were more frequently given psychotherapy and those from the lower classes were given ECT. Such a critique of the scientific objectivity of psychiatry fed into a climate of questioning how environment and illness interacted.
Psychiatry as a profession also turned to broader epidemiological questions through social research on the emergence of physical health issues. For example, the MHA published a study of Heyfield, a rural town in Gippsland, which covered both mental illness and certain physical conditions.[29] In Victoria, the Australian and New Zealand College of Psychiatrists also turned to social questions, with a ‘Political Issues Committee’ formed to develop positions on such controversial areas as abortion, homosexuality and capital punishment. Dax was encouraged to be the convenor ‘because he has shown considerable interest in the matter on both the social issues and the political issues side’.[30] Psychiatry was keen to expand its mandate and influence a range of broader social concerns.
There was, however, a countering phenomenon which threatened to undermine the validity of psychiatry. The anti-psychiatry movement played an important role in questioning the ability of psychiatrists to offer disinterested advice and some groups went so far as to claim that psychiatrists violated civil liberties.[31] Alongside this movement, there was an ascendancy of other groups who also claimed to represent a mental health industry, albeit one which saw itself as separate to, if not in opposition to, traditional psychiatry. These groups included social or welfare workers in community-managed organisations who worked directly with people diagnosed with psychiatric disorders, and who felt increasingly that people with mental illnesses should be involved in policy decisions. For example, Richmond Fellowship and the Schizophrenia Fellowship both became active in Victoria in 1977.[32] While the government files of groups such as the Victorian Association of Psychiatric Patients (VAPP), Psychiatric Complaints Council and the Campaign Against Psychiatric Injustice and Coercion (CAPIC) are closed to the public, it is clear that groups existed that began to speak from a critical perspective about psychiatry and treatment.[33]
Negotiating Boundaries: The Health Commission and Community Mental Health
In 1969, Cunningham Dax left Victoria for Tasmania and was succeeded by another psychiatrist, Alan Stoller. In 1975 the Health Commission was formed, integrating mental health under the broad umbrella of health.[34] The report which recommended the amalgamation of health services observed that mental health administration and its services had become too isolated. This foreshadowed the arrival of a multi-issue approach to health promotion which would attempt to incorporate mental health while also maintaining a separate policy area on community mental health services. This in turn saw psychiatrists developing specialisations in community treatment.
The Victorian Mental Hygiene Council (VMHC), an influential body in non-government mental health advocacy, took mental health to have ‘sociological, psychological, anthropological, spiritual, educational, biological and medical aspects’ in a letter it wrote to the Minister for Health in 1975.[35] Its wide definition meant that the tasks which were seen to be potentially related to ‘mental health’ could go far beyond the traditional medical treatment of psychiatric illness. In 1975 the VMHC’s members included ‘community leaders, teachers, clergymen, employers, housewives, retired people, office workers, doctors, nurses, psychologists, psychiatrists, and representatives of many agencies including social workers’. The group ran an Annual Prize known as the ‘Victorian Council for Mental Hygiene Cunningham Dax Prize’ which was ‘awarded for an essay on Mental Health in its broadest sense’. In 1973 the prize went to an essay on ‘The Survival of the Nuclear Family’. Alan Stoller, Chairman of the MHA, was asked by the Minister what he thought of the organisation and he wrote in a note that it should be supported.[36]
The Commonwealth Mental Health and Related Service Assistance Program in 1973 provided for eight new community mental health services in Victoria. These services posed challenges in determining how much support was required and how roles should be defined. For example, communities which abutted psychiatric hospitals feared that early release of patients may make them unsafe. A letter written in 1978 from Steve Crabb, MLA for Knox and signed by many local residents, complained about the early release of one patient who had been guilty of indecent assault, and stated that residents were frightened to go outdoors. During this period, community mental health required increasingly careful negotiation between government and community about what was deemed to be acceptable practice in terms of managing people with mental illness who were discharged from hospitals.[37]
The Health Department/Social Welfare Department Standing Committee provided one forum for this negotiation. In 1978 there were debates about how to manage people with mental illness who required services from the Social Welfare Department, with the committee deciding that it was not necessary to get the approval of the Head Office of the Mental Health Department to assess state wards. Its minutes noted that even though small reception centres were being developed in regional areas it was difficult to find psychiatrists. There were also practical issues to resolve about patient records. The committee decided that all medical records, including psychiatric problems and treatment, should be included in the one folder. It was noted, however, that ‘some officers of the Mental Hygiene Branch of the Health Department, insist that the psychiatric records are the responsibility of their Branch’.[38]
While the administrative borders were being negotiated, the profession of psychiatry was also continually questioning its role in the public policy debates. In 1983 there was a forum on ethics in psychiatric practice at which Dax spoke on the topic ‘Are we treating the wrong patients?’. Dax considered that the scope of psychiatry had to include all the social issues which were attended to under the 1977 Inquiry into Human Relationships. He observed that ‘the public mental health services may in the future have the major task of organising the care of the community’s chronic psychosocial needs. I therefore imagine the future mental health services to become “Departments of Social and Preventative Psychiatry”‘. He also cautioned that there would be ‘demarcation disputes if there [were] perceived to be a threat to invasion of the social field’[39] and pointed out that if psychiatry were to assume its responsibility in this field, there would be opposition to the ‘medical model’ and labelling. This caution was well-founded as voluntary groups became more organised and expressed strong views about their roles as advocates for people with mental illness.[40]
1980s Health Promotion and Mental Health Literacy
Mental health administration had become increasingly integrated within the bureaucratic structure of the Health Commission, consistent with the trend towards linking policy around mental health and generic health. This also applied to the area of health promotion. In 1980, a meeting of all the commissioners and divisional directors of Health made recommendations about how a sum of $50,000 should be allocated to health promotion. The Mental Health Division was included in this process. The aim of health promotion was to ‘raise people’s awareness that they can do things to improve their health and to reduce health costs’. A second aim was to ‘promote the corporate identity of the Health Commission of Victoria’ and establish favourable attitudes toward the commission. There were plans for a logo, slogan, jingle, posters and media coverage.[41] Health promotion was to be encouraged, and mental health was seen as part of the definition of health.
The concept of health promotion at this time was not unanimously endorsed within the bureaucracy, however. Patricia Mundy, from the Health Promotion Unit, wrote a memo to J Bennie, Convenor of the Health Promotion Committee, on the subject ‘What is meant by health promotion?’. She expressed concern that the commissioners and Health Promotion Committee did not understand health promotion the same way. She wrote that ‘the definition of Health Promotion implies a positive state of health, valuable in its own right’, which could be achieved by providing people with self-help information, helping people acquire the skills to use this information, and outlining the services available.[42] The Director, Building and Services Division had another view, stating that as far as they were concerned, people should be provided with ‘care and attention when something goes wrong rather than being helped to live a healthier life’.[43] Herein lay a dilemma for the government in deciding how to invest in health promotion. To what extent should health services, including mental health services, devote resources to people who are not actually ill?
In the area of mental health, as we saw from the early 1950s, there was an interest in improving mental health literacy. This had continued throughout the 1960s and 1970s. The Mental Health Division of the Health Commission had continued to have its own mental health education staff, with Rachelle Banchevska still leading government work in this area. In a remarkable similarity to the model which Dax had requested thirty years earlier, there were two health education workers (one of whom was Banchevska) and a stenographer/typist. In 1980, it was noted by JL Evans in his report for the Health Promotion Committee on health promotion that the mental health education role could be spread into a wider field, while recognising Banchevska’s role and status as a professional with twenty years’ experience. An integrated health promotion unit appeared to be the preferred model, with mental health operating within a larger administrative health bureaucracy.[44]
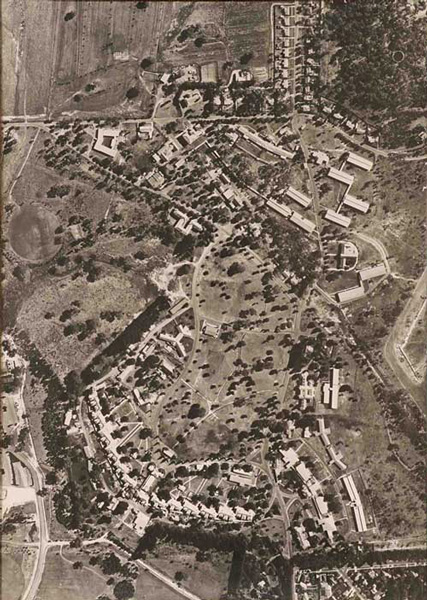
This approach was consistent with the move to treat people in the community and to improve the community’s mental health literacy. By 1986, with the passing of the new Mental Health Act 1986 (Vic) it was clear that the closure of the large psychiatric institutions was government policy. The money required to sustain these buildings and staff was greater than for community-based day services. The treatment preference was for ‘the least restrictive environment’ and the civil liberties of patients was to be more clearly enshrined in legislation. The report which recommended the closure of Willsmere Hospital, the former Kew Asylum, stipulated that budget requirements favoured this approach, alongside the social benefits of community-based services.[45] In the ten years from 1975 to 1985, 1600 beds were closed in Victoria and by 1985 there were 15 Community Mental Health Clinics and 17 Outpatient Clinics at hospitals.[46]
As mental health literacy was essential in this environment where people were to be treated outside of hospitals, psychiatrists saw an opportunity to apply for funds to run their own mental health education activities. In 1986 the Mental Health Foundation of Australia and the National Association of Mental Health sought funding from the Federal Minister for Health, Neal Blewett, to develop a community awareness program that discussed problems of mental health. In the same year, the Australian Government released a report on ‘The Better Health Commission’, which included just two paragraphs on mental disorders as one part of a much wider discussion of a health promotion program.[47]
Whilst the health promotion model was being developed and trialled, psychiatrists also looked at their own profession and found there was still a lack of unity in its approach. For example, the psychiatrist Graham Burrows, Chairman of the Mental Health Foundation of Australia, told the national conference of the Australian National Association for Mental Health in 1989, ‘We have to stop the silly fight, between psychology, sociology, psychiatry, medicine and physical health. The debate about whether it is psychological or biological must stop’.[48]
The late 1980s saw the further development of community organisations taking a leading role in defining how people with mental illness should be treated. Voluntary groups were given an even stronger role in service planning with the establishment of a peak body for psychiatric disability support services known as VICSERV, first funded in 1987. Its members were non-government agencies such as the North Eastern Alliance for the Mentally Ill (NEAMI) and the Outer East Council for Development of Mental Health Services, and offered alternative models of care. In the Melbourne suburb of Essendon, for example, there was an organised response from within the community to the establishment of a new community mental health service in 1989. A discussion paper on the topic reported that ‘new structures are developing and roles and responsibilities defined. There is still opportunity for new players to be involved and have an impact’. The paper warned however that bureaucratic constraints made input difficult: ‘The cumbersome nature of the operations of psychiatric services which place emphasis on the differences between professions and client confidentiality … can preclude co-ordination.’ Service providers were interested in the question ‘Where does decision-making power lie?’.[49]
By 1992, the state, territory and commonwealth governments had decided that a more co-ordinated approach to mental health issues was required. All governments agreed on a National Mental Health Policy which encouraged the states and territories to adopt a consistent approach to the treatment of mental illness, including the closure of stand-alone psychiatric hospitals. It also codified responsibilities for mental illness prevention and mental health promotion and applied the broad thinking about health promotion to the mental health sphere.
In 1993 the Human Rights and Equal Opportunity Commission released its Report of the National Inquiry into Human Rights of the Mentally Ill. This report focused on the experiences of people with mental illness and reflected a widespread recognition that the treatment, rehabilitation and social participation of people with mental illness since the advent of deinstitutionalisation had been below the standards of a caring society.
For the mental health industry, it could be argued that the last fifty years have seen an increased specialisation of professionals and a competition for resources and talented staff between the streams. The treating of people with mental illness in the public sector may have suffered a loss of status and, according to some, is now perceived to be the ‘second best’ stream within the profession.[50] While policy discussions over the last fifty years or so have revolved around the intention of reducing mental ill-health and suffering, it is debatable whether this goal has been reached, with research in 2001 finding that fewer than 40 per cent of people with mental disorders had received any care in a twelve-month period compared with almost 80 per cent for other common physical health problems.[51]
Mental Health, Psychiatric Language and Government Policy Differing concepts of mental health and mental illness have translated into robust debates about professional and policy roles and responsibilities. Government has been prepared to take leadership from psychiatry, while psychiatry has also had to adapt to the changing cultural landscape. The relationship between government and psychiatry has been even more complex because psychiatry itself has often been under the ‘conflicting influences of ideologies which are difficult to reconcile with each other and often contradictory’.[52] It has been argued that one of the reasons that psychiatry has struggled to find its role in the social debates about mental health is because as a profession it has lacked clarity about cause and treatment, especially the weightings it gives to biological or genetic, versus social or environmental, explanations.[53]
Moreover, the very definition of mental illness itself has evolved. The Diagnostic and statistical manual of the American Psychiatric Association, first published in 1952, was 100 pages long, while the fourth version, produced in 2000, is 943 pages. This explosion in the scale of psychiatry suggests that as forms of mental illness have multiplied, the expertise required to diagnose, differentiate and treat has also become more specialised.[54]
In 2002, the historian Roy Porter observed that the language of psychiatry had permeated Western culture, partly because the profession was unable to reach agreement about the role of medical and social factors in mental illness and treatment. Psychiatry:
still lacks the cognitive and professional unity enjoyed by general medicine and remains torn between bio-psychosocial and medical models both of its object and its therapeutic stages. Meanwhile, partly because of the proliferation of psychiatries, more people are said to be suffering – indeed claiming to be suffering – from a proliferation of psychiatric syndromes, in a ‘victim culture’ in which benefits may appear to lie in buying into psychiatric syndromes … as the idioms of the psychological and psychiatric replace Christianity and humanism as the ways of making sense of one’s self.[55]
This proliferation of psychiatric syndromes can be seen in the government policy tendency to slip between different medical and social constructs of mental health. It can be argued that government has been increasingly prepared to accept the role of community as a major defining element in mental illness, its prevention and treatment. This is at least partly because the individual with mental illness is no longer seen as an object to be incarcerated in a large stand-alone psychiatric institution, but rather as a subject who exists in an active relationship with his or her community. The current mental health policy now includes attention to the impact of mental health issues on the whole community.[56] Therefore the very quality of community has become a central concept in mental health policy and informs the thinking behind policy and service delivery.
Conclusion
The policy debates about mental health have been characterised by many different concepts and intended aims. In Victoria, there has been a move from a central Mental Hygiene Authority, with responsibility for all aspects of mental illness, treatment and education, to a more integrated concept of mental health with a multitude of stakeholders and perspectives. Objectives related to treatment have always been paramount in policy formulation, but increasingly the wider community has taken centre stage.
Psychiatric terminology entered the public arena through the influence of psychiatrists operating within government and also through the increasing advocacy of voluntary agencies. These struggles took place against a backdrop of new models of health promotion which gained ascendency in the public administration, and while psychiatry has influenced the formation of this model it has also had to adapt to the changing public policy context.
One of the key defining features of the policy context was the shift toward community care. While many files which relate to this issue are closed to the public, it is hoped that further research can be conducted to deepen our understanding of how policy evolved in relation to community mental health. This article has suggested that the closure of the psychiatric institutions required a greater focus on community education about mental illness to encourage people to recognise symptoms of illness and seek earlier treatment. This process posed challenges for psychiatry as it sought to define its various roles in both clinical treatment and the improvement in mental health literacy. Further research on the development of the different educational approaches and the evolving relationships between the various professionals involved will further advance our understanding of the complex area of mental health policy in Victoria and beyond.
Endnotes
[1] My thanks go to Sebastian Gurciullo at PROV and the two referees who provided very useful and constructive feedback on earlier drafts of this article.
[2] H Herman, S Saxena & R Moodie, Promoting mental health. Concepts. Evidence. Practice. A report of the World Health Organization, Department of Mental Health and Substance Abuse in collaboration with the Victorian Health Promotion Foundation and the University of Melbourne, World Health Organisation, Geneva, 2005.
[3] I Hickie et al., ‘Australian mental health reform: time for real outcomes’, Medical journal of Australia, vol. 182, no. 8, 18 April 2005, pp. 401-6.
[4] Cited in EB Brody, ‘The World Federation for Mental Health: its origins and contemporary relevance to WHO and WPA policies’, World Psychiatry, vol. 3, no. 1, February 2004, pp. 54-5.
[5] Minutes of Council Meetings of the Australian Association of Psychiatrists, 8 June 1948, Series 10, held at the Royal Australian and New Zealand College of Psychiatrists.
[6] WD Rubinstein & HL Rubinstein, Menders of the mind: a history of the Royal Australian and New Zealand College of Psychiatrists 1946-1996, Oxford University Press, Melbourne, 1996, p. 19.
[7] J Damousi, Freud in the Antipodes: a cultural history of psychoanalysis in Australia, University of New South Wales Press, Sydney, 2005, p. 249.
[8] Letter from Alexander Kennedy to CP Gartside, PROV, VA 629 Office of the Chief Parliamentary Counsel, (previously known as Parliamentary Draftsman, 1879 to 1970), VPRS 10265/P0 Parliamentary Counsel Bill Files, Unit 386 Mental Hygiene EB 298, 27 October 1949.
[9] PROV, VA 652 Health Commission of Victoria, VPRS 6345/P0 General Correspondence Files, Unit 28, Item 500/2 Pt. 2 Mental Hygiene – Appointment of Members.
[10] Age, 29 December 1951, p. 3.
[11] Argus, 20 July 1951, p. 2.
[12] Letter from EC Dax to WO Fulton, PROV, VPRS 6345/P0, Unit 421, Item 1094 Mental Health Advisory Committee Reports, 21 July 1952.
[13] Mental Hygiene Authority Annual Report, 1955, p. 7.
[14] EC Dax to Minister for Health, PROV, VPRS 6345/P0, Unit 86, Item 556 Mental Hygiene Information Bureau, 27 November 1952.
[15] EC Dax, Asylum to Community, Cheshire, Melbourne, 1961, pp. 185-7.
[16] Human Services Archives, Minutes of the Mental Hygiene Authority, 98/352/1, meeting held 2 November 1960.
[17] Dax, op. cit., p. 148.
[18] Mental Hygiene Authority Annual Report, 1959, p. 7.
[19] Dax, Asylum to Community, pp. 87-94.
[20] P Beilharz, M Considine & R Watts, Arguing about the welfare state: the Australian experience, Allen & Unwin, Sydney, 1992, p. 109.
[21] R Mendelsohn, ‘The Australian standard of living and the development of social welfare’, in K Hancock (ed.), The national income and social welfare, Cheshire, Melbourne, 1965, p. 35.
[22] C Syme & L Townsend, Report of the Committee of Inquiry into Hospital and Health Services in Victoria, Melbourne, 1975, p. 58.
[23] JFJ Cade, Mending the mind: a short history of twentieth century psychiatry, Sun Books, Melbourne, 1979, p. 50.
[24] ibid, p. 77.
[25] Royal Australian and New Zealand College of Psychiatrists (RANZCP) Archives, Minutes of meeting held 12 October 1959.
[26] G Rosen, Madness in society: chapters in the historical sociology of mental illness, Routledge & Kegan Paul, 1968, pp. 326-7.
[27] DA Hamburg (ed.), Psychiatry as a behavioural science, Prentice-Hill, Englewood Cliffs, NJ, 1970, p. 2.
[28] ibid., p. 36.
[29] J Krupinski et al., A community health survey of the rural town of Heyfield, Victoria, Australia, MHA, Melbourne, 1970.
[30] RANZCP archives, minutes of Council meeting 4 May 1969.
[31] N McConaghy, Liberation movements and psychiatry: Geigy Psychiatric Symposium, Ciba-Geigy, Sydney, 1974.
[32] A history of the Richmond Fellowship is available on the Mind Australia website, while the history of the Schizophrenia Fellowship can be found on the website of Mental Illness Fellowship Victoria (both accessed 30 August 2008).
[33] See PROV, VA 2838 Mental Hygiene Authority, VPRS 8787/P1 Alphabetical Subject Index to General Correspondence Files (Mental Health), Unit 1, which contains a file on the Victorian Association of Psychiatric Patients (81/181); Unit 2, which contains files on the Campaign Against Psychiatric Injustice (82/72) and the Patients Complaints Council (81/173).
[34] Syme & Townsend, op. cit.
[35] PROV, VPRS 6345/P0, Unit 470 Victorian Council on Mental Hygiene, File No. 2, letter from the Victorian Mental Hygiene Council to the Minister for Health, 8 July 1975.
[36] ibid., letter from David Fearon, President of the VMHC to Major General Sir Rohan Delacombe, 23 August 1971.
[37] Letter from Steve Crabb to VO Dickie, PROV, VPRS 6345/P0, Unit 369, Item 662/2 Larundel Mental Hospital General Correspondence, 19 June 1978.
[38] PROV, VPRS 6345/P0, Unit 536, Item 2109 Social Welfare Department – Inter Departmental Committee, Minutes of meeting of Health Department/Social Welfare Committee 25 October 1978.
[39] Dax, ‘Are we treating the wrong patients?’, in R Ball (ed.), Ethics in relation to psychiatric practice: proceedings of the conference, 1st July 1983, Fitzroy, Victoria, St Vincent’s Hospital, [1983], pp. 2-17.
[40] Advisory Committee on Volunteers, Volunteer and self-help groups in mental health and retardation fields: seminar October 3rd 1981, The Committee, Prahran, Victoria, 1981.
[41] PROV, VPRS 6345/P0, Unit 622, Item 81/174 Health Promotion, ‘Report on Working Party on Health Promotion’, 13 February 1981.
[42] ibid., memo from P Mundy to J Bennie, 25 February 1981.
[43] ibid., memo to Deputy Secretary, Health Commission, 20 February 1980.
[44] ibid., report by JL Evans on Health Promotion, 26 November 1980.
[45] Social Development Committee, Parliament of Victoria, Report Upon the Inquiry into the Future Use of Willsmere Hospital, Government Printer, Melbourne, 1985, pp. 95-100.
[46] ibid., p. 96.
[47] The Better Health Commission Interim Report, Canberra, Australian Government Publishing Service, 1986.
[48] G Burrows, ‘Mental health community awareness’, in The mental health status of the nation, Australian National Association for Mental Health, National Conference, 23 and 24 August 1988, pp. 17-20.
[49] PROV, VA 898 Essendon City, VPRS 12751/P1 General Correspondence Files, Multiple Number System, Unit 94, Item 315/1/16 Pt 1 Office of Psychiatric Services Mental Health Services, Community Mental Health Service in Essendon 1987-89, Discussion Paper ‘Community Mental Health Services’, 1 February 1989.
[50] Rubinstein & Rubinstein, op cit., p. 165.
[51] Hickie et al., op. cit., p. 401.
[52] P Pichot, A century of psychiatry, F Hoffmann-La Roche and Co., Basel, 1983, p. 177.
[53] A Scull, The insanity of place/the place of insanity: essays on the history of psychiatry, Routledge, London, 2006, see Chapter 9, ‘Psychiatry and social control in the nineteenth and twentieth centuries’.
[54] R Porter, Madness: a brief history, Oxford University Press, Oxford, 2002, p. 214.
[55] ibid., pp. 217-18.
[56] Department of Human Services, Because mental health matters. A new focus for mental health and wellbeing, consultation paper, Melbourne, 2008.
Material in the Public Record Office Victoria archival collection contains words and descriptions that reflect attitudes and government policies at different times which may be insensitive and upsetting
Aboriginal and Torres Strait Islander Peoples should be aware the collection and website may contain images, voices and names of deceased persons.
PROV provides advice to researchers wishing to access, publish or re-use records about Aboriginal Peoples
